Optimising skin cancer pathways through digital transformation with PathpointⓇ eDerma

eDerma is an award-winning, cloud-based digital solution designed for dermatology service coordination. Developed by NHS clinicians and in collaboration with dermatologists and patients, it represents true innovation. Its success stems from its remarkable flexibility, seamlessly integrating into existing workflows and catering to specific community needs.
This adaptability efficiently addresses the resource constraints in UK dermatology, making the most of limited time and resources. Notably, eDerma includes a patient questionnaire co-designed with both dermatologists and patients, enhancing patient accessibility and understanding to improve referral quality and patient assessments. Moreover, by integrating with legacy and modern hospital systems, it ensures continuous care, minimising fragmentation. With its unique approach, eDerma delivers maximum benefits to patients and service users, proving to be a transformative solution in dermatology service coordination.
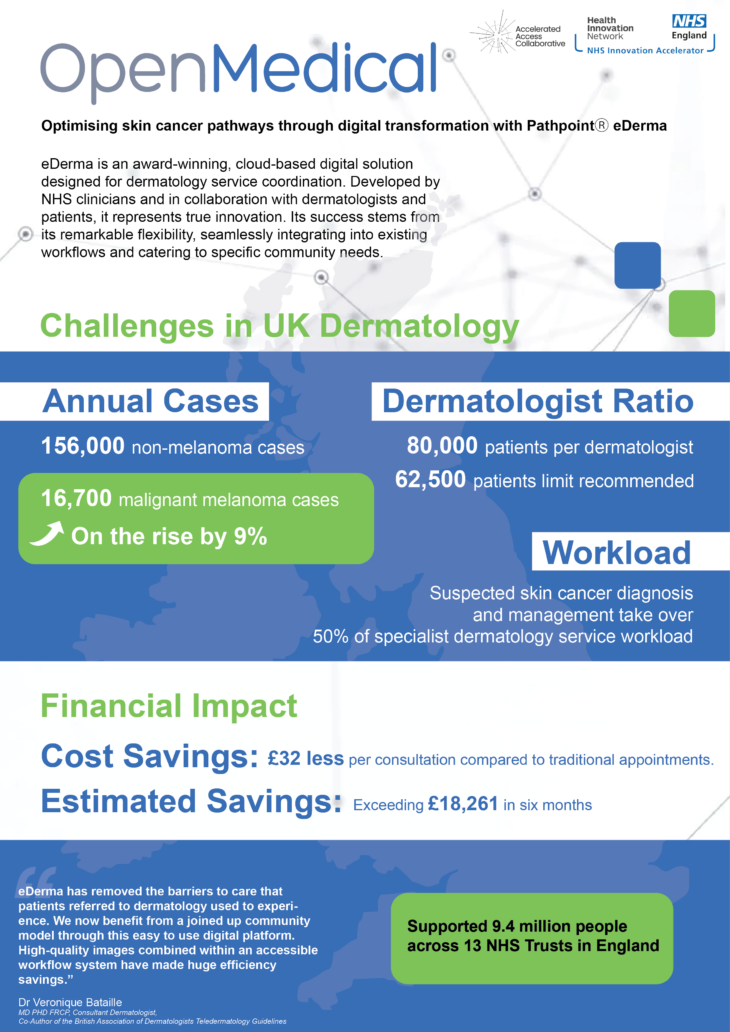
In the UK, there are around 156,000 non-melanoma and 16,700 malignant melanoma cases annually, projected to rise by 9%. Limited dermatologists and patient access create challenges in meeting faster diagnostic standards, causing delays in treatment. In the UK, each dermatologist is responsible for approximately 80,000 people, well above the recommended 62,500 limit.
The diagnosis and management of suspected skin cancer takes over 50% of a specialist dermatology service workload and timely diagnosis is crucial for cancer survival rates.
Collaborating with the NHS Innovation Accelerator (NIA) and the Small Business Research Initiative (SBRI) Healthcare, Open Medical has joined forces with NHS Trusts and Integrated Care Systems (ICSs) to revamp and enhance their teledermatology pathways. This transformative initiative leverages Open Medical’s digital solution, PathpointⓇ eDerma, to streamline and improve the efficiency of dermatology services. This collaboration allowed the healthcare institutions to overcome resource limitations and significantly reduce the time from referral to diagnosis for patients with suspected skin cancer. These projects not only improved efficiency and care for patients but also proved to be cost-effective, increased accessibility, and addressed health inequalities. The success of these projects has led to plans for implementation across other ICSs and hospitals and the expansion of eDerma’s reach, with the aim of sharing learnings nationally and globally.
Open Medical boasts a PPIE committee integral to crafting patient questionnaires for eDerma, resulting in a commendable 99% completion rate prior to teledermatology appointments, with patients finding it notably user-friendly. The participants’ valuable feedback significantly influenced the project, with a thorough interview process showcasing their contributions being valued and accepted at a rate of 90%. This collaboration fostered skill development within both the Open Medical team and the PPIE participants, leading for valuable lessons to reflect back on. The engagement of patients and the public in the project positively impacted product development, data analysis, and the creation of patient-facing materials.
In summary, the financial impact of eDerma has been impressive, with each consultation costing £32 less than traditional face-to-face appointments, resulting in significant savings. Independent evaluations estimated potential savings exceeding £18,261 in just six months compared to the previous pathway, emphasising its cost-effectiveness. The teledermatology model demonstrates efficiency, boasting referral-to-assessment times under one week, 99% first seen within two weeks, and assessments completed in an average of approximately 5.5 minutes – up to four times faster than face-to-face appointments, thus increasing dermatologist capacity. Notable achievements include substantial reductions in face-to-face appointments, addressing health inequalities, direct bookings for diagnostic biopsies, and high patient satisfaction. eDerma currently supports a population of 9.4 million across 13 NHS Trusts in England, with plans for further expansion in 2024 across the UK and globally, including launches in two Integrated Care Systems in Q1, 2024.
Dr Veronique Bataille MD PHD FRCP, Consultant Dermatologist, Co-Author of the British Association of Dermatologists Teledermatology Guidelines, said:
“eDerma has removed the barriers to care that patients referred to dermatology used to experience. We now benefit from a joined up community model through this easy to use digital platform. High-quality images combined within an accessible workflow system have made huge efficiency savings.”